Abstract

Background:
The role of radiation therapy (XRT) in patients (pts) with advanced stage diffuse large B-cell lymphoma (DLBCL) remains controversial. Locoregional XRT is often recommended to pts with less than a complete response (CR) on computerized tomography (CT) and to those with bulky disease at diagnosis. Selective administration of XRT guided by functional imaging at end-of-chemotherapy-treatment (EOT) may spare pts XRT if they are PET negative (PET-neg), and facilitate eradication of a residual chemo-resistant site in those with a positive scan (PET-pos).
Methods:
Since July 2005, pts with advanced stage DLBCL (stage 2 with B symptoms and/or bulky disease, stage 3-4) treated in British Columbia (BC) have been recommended to have a PET if they have a residual mass > 2cm on the EOT CT scan, although some pts do proceed to PET without documented residual masses on EOT CT at the discretion of the treating physician. XRT (to the involved site) was offered to pts with PET-pos residual disease provided the area of persistent PET positivity could be encompassed within a reasonable radiation volume. Pts with a negative scan (PET-neg) were observed, regardless of initial bulk or original disease sites. The BC Cancer Agency Lymphoid Cancer Database and Department of Functional Imaging database were used to identify all advanced stage, newly diagnosed DLBCL pts treated with a minimum of 6 cycles of RCHOP between Jan 2005 and Oct 2016 that had an EOT-PET scan. This analysis did not include pts with documented progressive disease during RCHOP, known CNS involvement at diagnosis, HIV positivity, primary mediastinal large B-cell lymphoma, transformed lymphoma, or those treated with XRT prior to completing RCHOP. All PET scans in BC are performed in a single location using a combined PET/CT scanner with centralised review. Scans performed prior to the introduction of the Deauville criteria were reported as per the recommendations of the International Harmonisation Project.
Results:
702 newly diagnosed DLBCL pts were identified with the following baseline characteristics: median age 65 y (range 18-87 y), 57% male, 43% PS >1, 58% elevated LDH, 30% >1 extranodal site, 74% Stage III/IV, 40% bulky site ≥10cm, 43% IPI 0-2, 57% IPI 3-5. Only 6% of included pts received >6 cycles RCHOP. Median follow up for living pts was 3.3y (0.3-12 y).
498 (71%) pts were PET-neg at EOT and 204 (29%) PET-pos. 109 (53%) PET-pos pts were treated with XRT, 95 (47%) were not. Reasons for not receiving XRT: 1 refused, 8 had surgical resection of their FDG-avid site (x7 splenectomy, x1 mastectomy) and 23 were selected for close observation by the treating physician. 63 were not referred for consolidative XRT as the location or extent of PET-pos sites were deemed not amenable to XRT or they had clear evidence of disease progression. These pts were referred for additional systemic treatment or palliation. Only 4 PET-neg pts were treated with XRT at the discretion of their treating physician. Most pts were treated with 35 Gray (range 30-45) delivered over 20 fractions (range 10-25) depending on site and field.
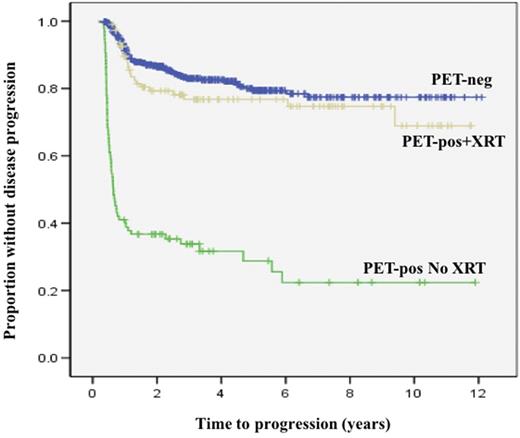
5-y time to progression (TTP) and overall survival (OS) were similar for both PET-neg pts (79% and 82%, respectively) and PET-pos pts who received XRT (77% and 73%, respectively). PET-pos pts who did not receive XRT had inferior outcomes (5-y TTP 29%, 5-y OS 43%).
Within the entire cohort, 272 had a documented bulky site of ≥10cm at diagnosis. 161/272 (59%) pts with original bulky disease were PET-neg at EOT and therefore not treated with XRT. No significant differences were observed for TTP or OS in PET-neg pts who had bulky vs non-bulky disease at diagnosis, regardless of definition of bulk used (≥ 7.5 cm or ≥ 10 cm).
24/109 (22%) pts in the PET-pos cohort who were treated with consolidative XRT relapsed: 7 out-of-field, 4 in-field, 12 in- and out-of-field, 1 unknown. There is a cohort of 29 pts with PET-pos disease who received no further treatment and have not had documented disease progression.
Conclusion:
This population-based analysis with long-term follow-up confirms that using a PET-directed approach to guide the use of XRT can spare pts from potential adverse effects of XRT without compromising outcome. The outcome of pts with PET-negative disease is comparable with previously published series and not significantly different from those with PET-pos disease who were treated with XRT. Among pts with bulky disease at diagnosis, almost 60% can be safely spared XRT.
Freeman: Seattle Genetics: Honoraria; Roche/Genentech: Research Funding; Abbvie: Honoraria. Savage: Celgene: Consultancy; Roche: Research Funding; Seattle Genetics: Consultancy, Honoraria; Bristol-Myers Squibb: Honoraria; Merck: Honoraria. Villa: Seattle Genetics: Consultancy, Honoraria; Lundbeck: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Abbvie: Honoraria; Celgene: Consultancy, Honoraria; Roche: Consultancy, Honoraria. Scott: Celgene: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; BCCA: Patents & Royalties: Patent describing molecular subtyping of DLBCL licensed to NanoString Technologies. Patent describing measurement of the proliferation signature in MCL.. Gerrie: Lundbeck: Honoraria; Janssen: Membership on an entity's Board of Directors or advisory committees; Roche: Research Funding; Seattle Genetics: Honoraria, Membership on an entity's Board of Directors or advisory committees. Slack: Seattle Genetics: Consultancy. Connors: Amgen: Research Funding; Lilly: Research Funding; Janssen: Research Funding; NanoString Technologies, Amgen, Bayer, BMS, Cephalon, Roche, Genentech, Janssen, Lilly, Merck, Seattle Genetics, Takeda,: Research Funding; F Hoffmann-La Roche: Research Funding; Cephalon: Research Funding; Genentech: Research Funding; Bayer Healthcare: Research Funding; Bristol-Myers Squibb: Research Funding; Seattle Genetics: Research Funding; NanoString Technologies: Research Funding; Merck: Research Funding; Takeda: Research Funding. Sehn: Seattle Genetics: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Roche/Genentech: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Amgen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal